Papa is a first-of-its-kind solution using technology to deploy personalized, community-level care to older adults, underserved populations, and families at scale. Learn more about our offerings below.
A New Kind of Care

The Papa platform
We do what technology alone cannot—provide members with real human connection and support to address health-related social needs, provide respite for family caregivers, and advance health plan quality objectives. Here’s how we do it.
National network of Papa Pals
Best-in-class technology platform
World-class operations
Engagement pathways
Solutions & offerings

Core Companionship
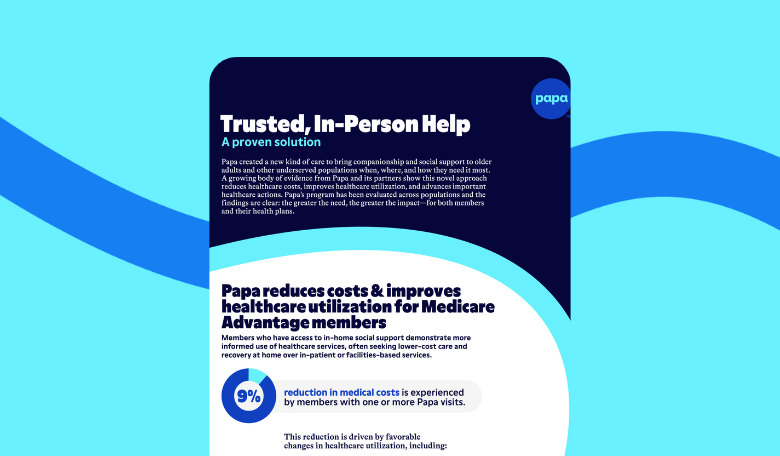
Papa’s legacy companion care model provides personalized, hyper-local support on a national scale. Available in person or telephonically, our vetted Papa Pals address the root social needs that impact your members’ health and well-being, like rides to the grocery store or pharmacy, help around the house, social interaction and companionship, and much more. Papa can work with you to tailor enrollment so we reach the members who need us most—generating the greatest impact and highest savings. Review our health plan page for more information on how Papa can benefit your population.

Papa provides employees with a reliable source of assistance and an extra set of hands during life’s challenging moments—helping them care for aging or ill loved ones, children, or themselves. Papa’s national network of highly vetted Papa Pals meets employees and their families exactly where they are, offering personalized, human help unbounded by the limitations of traditional programs or infrastructure. Papa Pals serve as companions for aging or ill loved ones when employees can’t be there themselves, parents’ helpers while employees finish the work day or juggle other tasks, added reinforcement during life events, like a hospitalization or birth of a child, and much more. Papa is not another digital front door; we’re help to the front door however employees need it most. Review our employer page for more information on how Papa can benefit your employees.

Papa Plus integrates companion care with targeted quality programs, transforming in-home support into a direct, outcomes-oriented engagement channel for health plans. With Papa Plus, trusted Papa Pals provide member-directed support for everyday needs, while also supporting plan-directed tasks to drive measurable outcomes across quality ratings, healthcare utilization, member satisfaction, and retention, for a guaranteed ROI.

Health plans can add post-discharge support to companion care or leverage it as a standalone program to ensure members transitioning home from a hospitalization receive an extra layer of support. Papa Pals fill gaps in social support to enable recovery at home, encourage discharge plan adherence, and optimize utilization of plan benefits to ultimately reduce avoidable readmissions.

Health plans can add care gap closure support to companion care or leverage it as a standalone program. Trusted Papa Pals provide in-person support with scheduling, door-through- door transportation, and encouragement to help members complete critical preventive care and improve quality ratings.

Health plans can add digital enablement to companion care or leverage it as a standalone program to bridge the care access gap and advance digital health adoption. Members complete an assessment and receive in-person help from Papa Pals to learn and gain comfort with member portals, telehealth, pharmacy and benefit apps, and more.

Papa transforms Health Risk Assessment (HRA) completion from an inefficient transaction into a simple, flexible, and trusted process. We meet members on their terms—conducting the HRA in our standard enrollment process or connecting members who need more help with in-person Papa Pals to complete it. This multi-modal approach drives higher completion rates by deploying the right level of support to the right member, ensuring no one is left behind, while uncovering valuable member insights in the process.
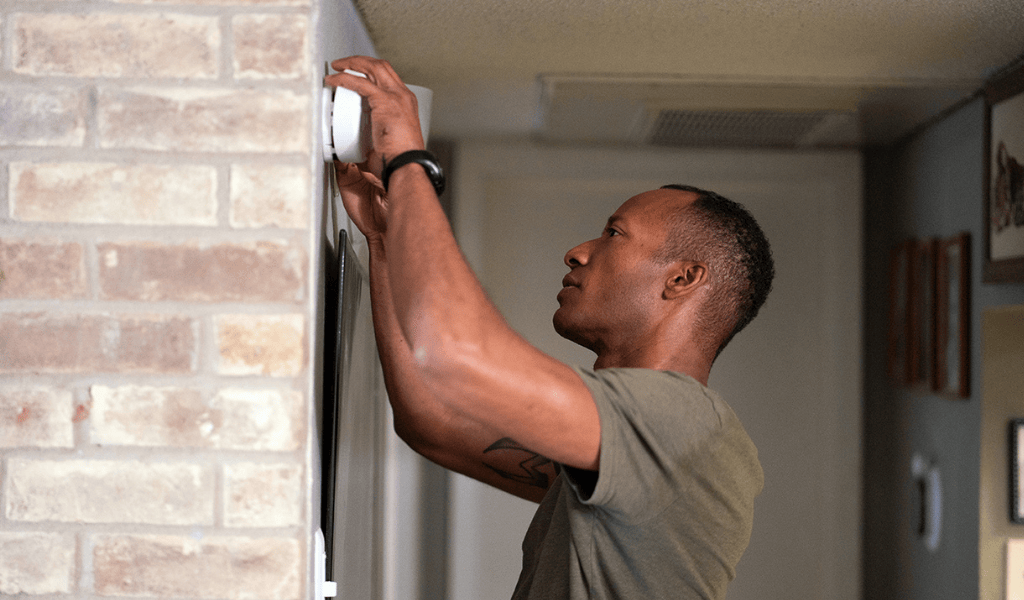
Papa Pals as eyes and ears in the home. With Papa’s Fall Risk Prevention program, which can be added to core companion care or leveraged as a standalone service, Papa Pals conduct a Home Safety Assessment (HSA) to identify and report on home environment and potential hazards. Papa can also help connect members to necessary services based on uncovered needs to help make their homes safer.