Papa’s digital health literacy offering bridges the care access gap. It also addresses a new CMS health equity requirement for Medicare Advantage plans to identify and offer digital health education to members with low digital health literacy.
Digital Health Literacy

A proven solution
Papa has long supported members with technology assistance. In fact, Papa Pals have successfully completed more than 67,000 technology visits with Medicare Advantage members since January 2022. Papa has now layered on specific tasks related to CMS’ goal of improving virtual care access for dual-eligible, disadvantaged, and low-income members. With this enhanced service, Papa assesses, addresses, and reports on a range of digital health literacy needs to help health plans improve member access to quality health care. Here’s how it works:
Assess
Papa’s Care Center conducts an initial social needs assessment for each member that evaluates digital health literacy, internet access, and more.
Schedule in-home visit
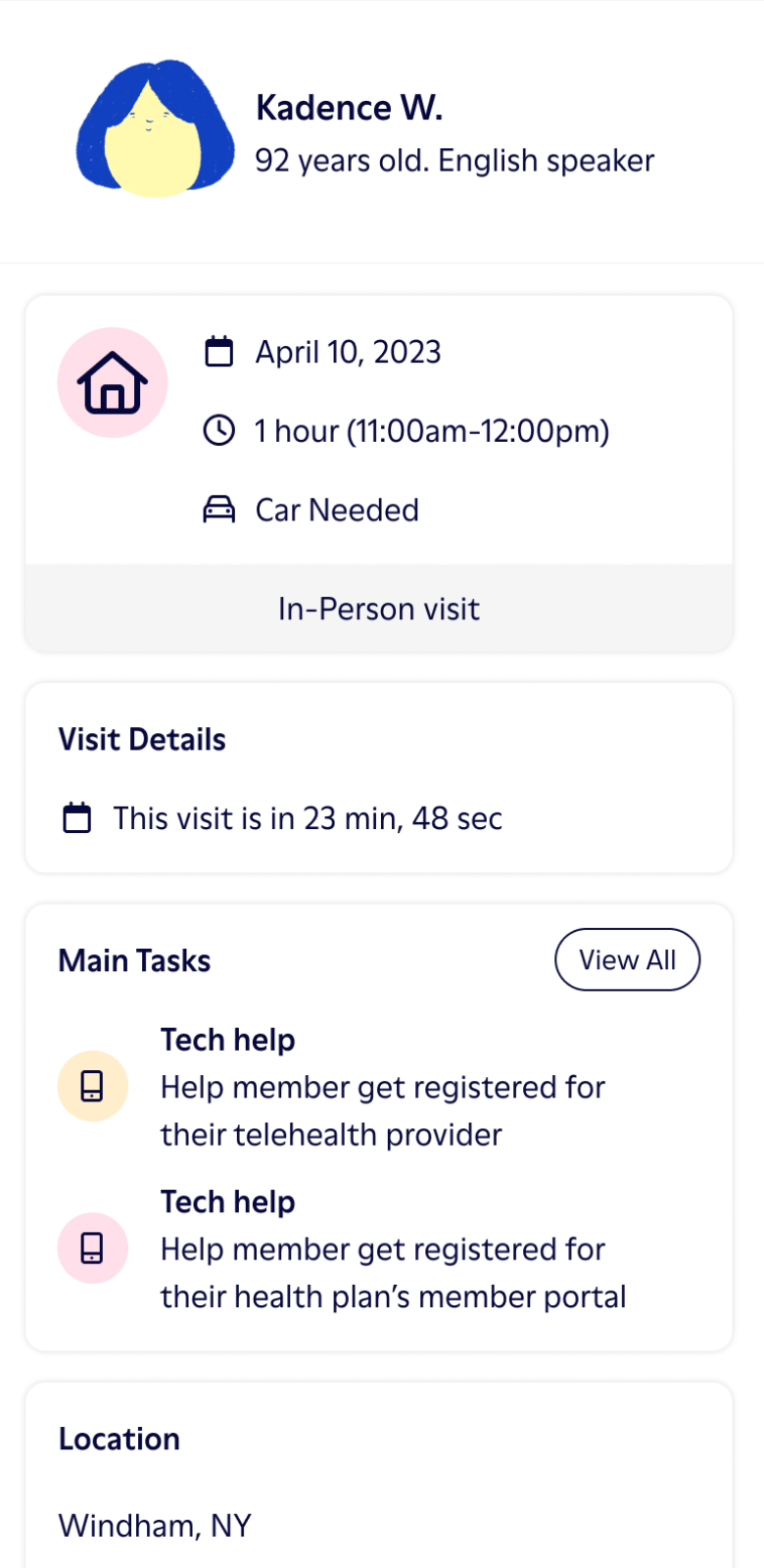
Visits are scheduled for Papa Pals to meet with members and help with specific tasks. Papa Pals are available nationally and leverage existing relationships with members to provide trusted one-on-one support.
Conduct in-person visit
Papa Pals travel to members’ homes for education and support with digital health training and specific technology tasks, such as helping members set up and learn to use their health portal or telehealth services.
Follow up
Social care navigators follow up with members after their visit to see if their digital health needs were resolved. Navigators can schedule additional Papa Pal visits or connect members to health plan or community resources as needed to ensure their needs are met.
Report
Papa provides robust reporting at every step—from initial screenings to member needs to resolution confirmation—so health plans can know more about their members’ digital health literacy needs and monitor improvements.

A real person drives real value
Papa’s solution allows for a purpose-built network of Papa Pals to leverage existing, trusted relationships with members to help educate and enable them to gain the digital skills they lack today.
Market gap
40%
A need for in-person help
73%
Low utilization
97%
Potential cost savings
6%
Interested in Papa for your members?
Do you work for a health plan and are interested in offering Papa to your members?
Want to learn more about how our Digital Health Literacy impact program can work for you? Let’s chat!
*Papa presently does not provide services directly to individual consumers. Please be aware that responses to this form submission are intended solely for inquiries from health plan organizations. Any other inquiries will not receive a response.


