Health plans, networks, and providers offer a variety of social isolation care plan options and keep close tabs on how member health outcomes measure up. They work consistently to improve both quality of care and member experience. While all players recognize the value of social isolation prevention, reaching people with effective preventative measures is often a harder nut to crack.
Historically, much of the discussion around social isolation has revolved around screenings, wellness checks, healthy lifestyle habits, etc.–all of which are critical to heading off chronic disease and catching problems early. Social drivers of health, however, have become an important part of the prevention conversation.
One driver in particular, social and community context, is proving to have a big impact on whether some common health problems–heart disease, stroke, and mental illness–emerge and gain traction.
Social isolation vs loneliness
Social isolation vs loneliness are similar, but not one and the same thing.
Social isolation can affect individuals and entire families when they lack community context–consistent, meaningful support and connection from their community, and a sense of belonging. Loneliness is the feeling of being separate from, and even unnoticed by others (even if there are people around) and the absence of rewarding social relationships.
Both conditions increase the risk of mortality. In fact, according to the Campaign to End Loneliness, loneliness increases the risk of mortality from all causes by 26%.
And while over one-third of all Americans report serious loneliness, members of the population served by Medicare Advantage plans may be even more susceptible to health problems associated with loneliness because other social drivers of health (like economic stability, education access and physical environment) play an outsize role.
Among the chronic illnesses linked to social isolation are heart disease and stroke. Heart disease risk grows by 29%, and stroke risk goes up 32%.
Effects of social isolation
As Medicare Advantage plans strive to serve their members’ healthcare needs, the “big” chronic illnesses like heart disease, stroke, and diabetes absorb plenty of attention–and resources.
When social isolation and loneliness are issues, however, the risk of mental health problems also rises. Any social isolation care plan need to take the following into consideration. Stress caused by lack of companionship and social context can often bring on depression and anxiety. Among socially isolated people, 63% are either clinically depressed or suffer from debilitating anxiety, according to CDC data.
In turn, both depression and anxiety could predispose those who suffer from them to a range of illnesses. Depressed and/or anxious people may have reduced immunity to common infections like colds and flu, and be less inclined (or able) to take steps that might help them get better, such as eating a healthy diet or getting enough sleep. And depressed immunity opens the door to other more serious conditions.
In addition, people experiencing depression and anxiety often wait longer to seek medical care, if they seek it at all. And they are less able to care for family members, which can similarly lead to delays in essential medical care.
Social isolation can make people less safe in their homes
We’re well aware that the risk of in-home accidents rises for older people living alone, especially if they lack helpful connections with the outside community.
But younger people–and families–who may be socially isolated for any number of reasons, also face higher accident risk. Any successful social isolation care plan will address the absence of support from friends and extended family. This means the absence of another set of caring eyes and helpful hands to notice obvious hazards.
Lonely individuals can slip into a pattern where it’s just too much for them to keep up with healthy habits, and may be less able to fix in-home hazards on their own. And they might not notice subtle signs of their own deteriorating health.
Similarly, overwhelmed parents and caregivers often put their own health concerns on hold, or ignore them altogether to focus on the rest of the household. Sometimes the effort to just get food on the table is all they can manage, and other problems–like unsafe conditions in the home–get put off for another day.
Can the effects of social isolation be reversed?
Whether it’s concerns about chronic illness, mental health, or safety risks, adding a layer person-to-person care to create social support can turn around the lives of people who are lonely and/or socially isolated.
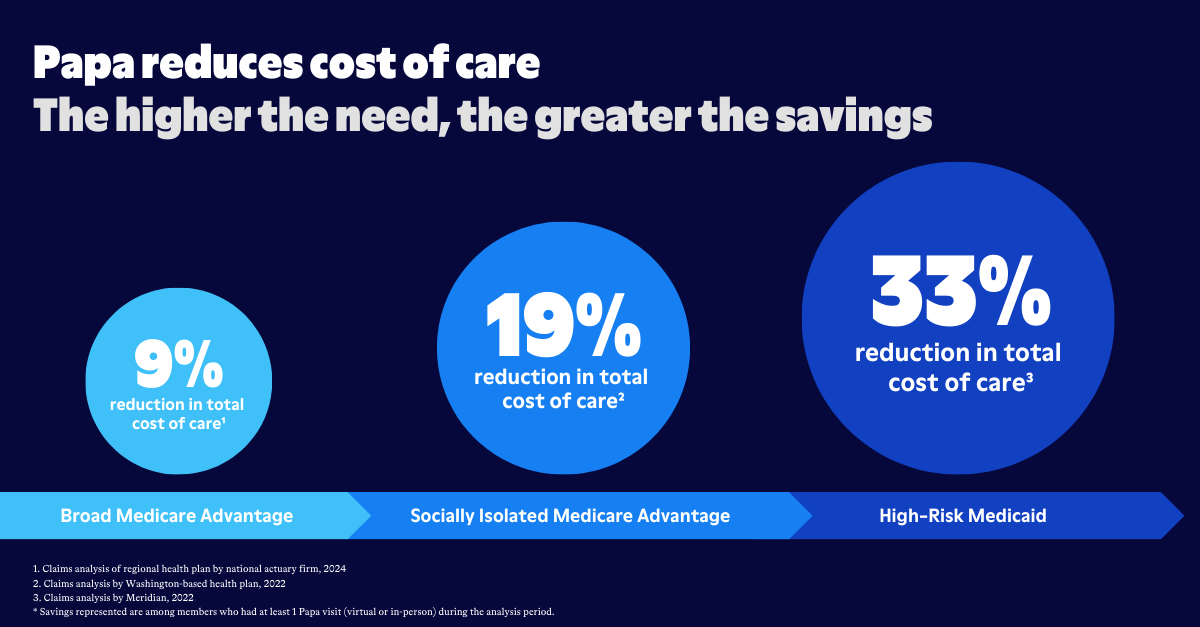
First up, a consistent and positive social context should be part of any social isolation care plan and can improve overall health and reduce mortality. It can also contribute to happier and healthier lives for individuals and families who have suffered from social isolation. And while “happier” may be a subjective measure, “healthier” can save money on many fronts: According to the AARP, $6.7 billion in annual spending is tied to social isolation.

Social support in the form of companion care, such as that offered by Papa Pals and other programs, can introduce cost-effective prevention to head off chronic illness, mental health problems, and accidents in the home.
Regular interaction with caring person from the outside can bring eyes and ears into the home to flag possible health concerns before they become more serious problem, or even turn into an emergency. Companion care can also help identify safety risks in the home such a tripping hazard, a faulty electrical outlet, a broken stair, or other dangerous conditions.
Just as important, companion care can bring on-the-spot assistance for simple tasks that might inadvertently cause a fall or other injury for someone attempting such tasks on their own. And companion care can help with check-ins, reminders, and transportation for regular healthcare visits.
Improve health outcomes one social connection at a time
The data makes one thing clear: People need people.
At Papa, we understand that there are many factors involved in a person's overall health. We know that there is not one clear defining factor that leads to poor health-- and not one clear panacea that improves health outcomes.
That said, we also recognize that health plans are always looking for ways to improve overall health outcomes and member experience, and by giving members access to companion care, health plans can help their members to be healthier.
One social connection at a time.