At Papa, we love people. All people.
And we want all people to thrive, which is why we are always thinking about solutions.
We look for solutions to help older adults live safely in the homes where they have made so many memories. We want them to be able to enjoy their golden years–to take exercise classes, to visit friends, to play BINGO in the community center on Friday nights.
We think about solutions to help sticky-fingered kids to embrace their childhoods and grab onto their potential. We want every single child to have the opportunity to paint pictures, ride bikes, visit friends, and learn algebra in safe homes in safe neighborhoods with plenty of food.
We strive to find solutions for the young, for the old, and for every member of the sandwich generation in-between. We want to find solutions that preserve health, solutions that help people who are sick, solutions that mitigate loneliness, and (of course), solutions that make a difference.
Health plans are taking strides to improve equity
Last month, we hosted a webinar about how health plans can improve lives and health outcomes for older members. Our guest for the webinar was Kathy Feeny, the CEO of Florida Blue Medicare. During the webinar, Kathy said something that really got us thinking.
She said, “We think of ourselves as a solutions company. Our values are baked into our DNA and baked into everything we do with our members. One that particularly stands out in our values and you’re going to hear me say this word is inclusion. Every individual needs to be included in terms of being able to have access to care, affordability, and having a usable plan. It needs to be a level playing field for all.” (If you want to hear everything she said about member inclusion, it starts at the 7 minute mark of the webinar.)
We loved hearing that one of our most trusted partners (Florida Blue) has values that so closely align with ours. We also loved what Kathy had to say about inclusion. In the days since, we’ve been contemplating what member inclusion means, and how we can come up with solutions that drive member inclusion to support both our partner health plans and our own members.
This is a learning process–for us and for everyone–but we thought we would share what we’ve learned so far.
What is member inclusion?
Member inclusion on the surface is simple: It simply means that each and every member has access to the health care services that they need to be healthy. But when we started unpacking that, the concept of member inclusion started to become a bit more complex.
For example, the health services that people need to be healthy include a whole lot more than doctor’s appointments and pharmacy benefits.
In the webinar, Kathy Feeny explained that Florida Blue has been focusing on adding supplemental benefit solutions to their plans in order to increase member inclusion. They offer all sorts of solutions, including Papa’s companion care, mental health benefits, brick-and-mortar health clinics and even a Silver Sneakers exercise program.
All of these programs give their members access to the solutions they need to be healthy.
Removing barriers to care
There is more to member inclusion than just offering programs. It also includes removing barriers to care. This means making sure that all members can get the care they need by making sure they have the transportation they need to get to health care visits, that they can afford to pay their co-pays and deductibles, and that qualified health care professionals are in every community and neighborhood. Removing these barriers to care makes a huge impact in member inclusion.
Removing barriers to care is one of our most important missions at Papa.
Our Papa Pals offer transportation to and from doctor’s appointments, and rides to pharmacies to pick up medications. They also offer companionship, help with errands, help finding and preparing nutritious food and childcare. These are simple solutions that remove barriers to care.
We want to go beyond “simple solutions” so we have been thinking about other ways that Papa can provide solutions for member inclusion.
Things like providing help with technology so that all members can access their benefits, or providing safety checks in homes to make sure members are safe are small steps that remove barriers to health.
Member inclusion leads to health equity and member engagement

Historically, health care hasn’t exactly been inclusive.
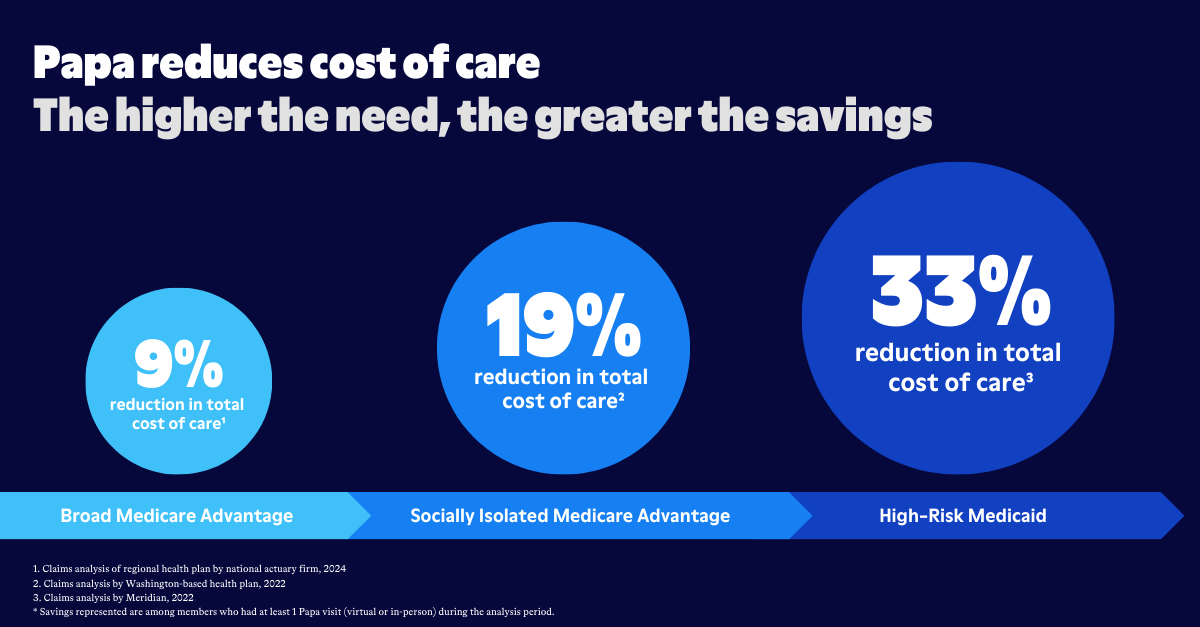
Systemic disparities in health care have long impacted members, and solutions for member inclusion were often neglected. But recent research into the cost of health inequity has changed that.
When all people don’t have access to the programs, benefits and health care providers they need, everyone suffers.
Those individual members suffer.
Their communities suffer.
Their health care providers suffer.
And yes, the health plans who insure them also suffer.
Care gaps are costly–both financially and in human terms. Plans now know that by being inclusive and by ensuring that all members have access to the health care solutions they need, they can improve health equity, and ultimately increase member engagement.
Papa Pals as a solution for member inclusion
Papa wants to support its health plan partners to find solutions for member inclusion.
When Kathy Feeny described the “bag of tricks” that Florida Blue uses to support member inclusion, she described the work Papa does with companion care to be her “most important service”.
That made us at Papa really happy– because our mission is to make sure no one has to go it alone. But it also got us thinking about how we can drive solutions for health inequality.
We want to help health plans engage each and every member who needs support, and we hope to do it through careful thought leadership and some creative solutions that get to the heart of what people need most.
Hint: the answer is other people.