What do Medicaid health plans really do?
Of course, Medicaid health plans provide health care to millions of Americans, ensuring that they have access to the health care they need and deserve. But recently, especially during and after the pandemic, Medicaid health plans have grown into so much more than just health care payers.
In the past several years, Medicaid health plans have grown into organizations that support entire communities through social interventions, preventive programs, education, and much more. Since the beginning of the COVID-19 pandemic, Medicaid health plans have expanded their social support services in innovative ways. These plans are addressing the social factors that impact health—social determinants of health—as they listen to what communities want and need. What’s more, they’re creating sustainable ways to provide this essential health care support.
Read on to learn about some of the most promising innovations in Medicaid health plans.
Medicaid health plans then and now
Medicaid was established in 1965. Children’s Health Insurance Program (CHIP) was created in 1997. In 2019, Medicaid and CHIP covered 71 million people combined. Our country’s most vulnerable populations are being served and cared for by Medicaid health plans.
The COVID-19 pandemic dealt a devastating blow to our health care system, economy, and the quality of life for all Americans—especially older adults, individuals with underlying health conditions, and communities of color.
The good news: Medicaid health plans have risen to the challenge and have pivoted their services and support to provide high-quality care to the people who need it most during this public health emergency.
Outpatient health care came to a grinding halt in early 2020 as much of the country shut down in response to COVID-19. Medicaid health plans stepped up to the plate to partner with communities to provide urgent health care in new ways. In 2021, the Institute for Medicaid Innovation (IMI) “conducted a national environmental scan to collect best practices of initiatives focused on meeting health and social needs to address inequities that were exacerbated by the pandemic". They compiled their findings into a report entitled Medicaid Managed Care’s Pandemic Pivot: Addressing Social Determinants of Health to Improve Health Equity. The report includes 33 initiatives from 14 states.
Let’s look at a few of them.
Enhancing maternal health in Texas

A health plan in Texas that serves children, teens, and pregnant individuals partnered with an organization that identifies individuals who need support. They offered connection to resources through a mobile app. This pilot partnership helped address the needs of the health plan’s pregnant members through the pandemic. Using a chatbot, the app connects members with individuals who listen without judgment, direct them to appropriate care, and educate them about benefits.
As of December 2021, 700+ pregnant members downloaded and used the app and more than half of them completed one or more behavioral health screenings. Almost 25% engaged with an agent to find resources and 10% used the app daily. The pandemic took a toll on pregnant members who often felt isolated and lonely and/or at risk for postpartum depression. The app helped identify those who might not have reached out otherwise and got them the support they needed.
A COVID-19 response plan in Michigan
One health plan in Michigan partnered with social service, religious, educational, and other organizations to educate communities about COVID-19 and the vaccine. Residents had expressed fear about the vaccine, especially after the widespread lead exposure and water crisis in Flint. The health plan set out to alleviate those fears through information and education.
The health plan created customized vaccine education for various at risk groups like young mothers and working adults. They offered incentives and home testing and set up drive-through vaccination events at local churches, businesses, and community centers. Beyond vaccination, they connected members to local food pantries and offered transportation to local grocery stores.
Providing employment in Pennsylvania

Roughly 9.6 million U.S. Americans lost their jobs due to COVID-19. Employment as a social determinant of health (SDoH) is an urgent concern for Medicaid health plans working to eliminate inequity. Equity isn’t possible without access to jobs with fair pay.
One health plan in Pennsylvania launched an initiative to provide training, education, and direct support to increase access to employment for their members who had lost jobs due to COVID-19. In response to the need for a more substantial and diverse paramedic workforce, they offered emergency first responder career training and provided job placement for members. The 10-week training program included a monthly stipend, childcare, access to a food pantry, and other benefits. Upon completion of the program, students were eligible for careers as community health workers or EMTs.
As of June 2022, they’ve had 21 students graduate from the program, 15 of whom are BIPOC (Black, Indigenous, or People of Color). There’s an 85% employment rate for graduates and they make an average of $15.60/hour in a state (PA) where the minimum wage is $7.25/hour.
Other promising initiatives… including Papa!
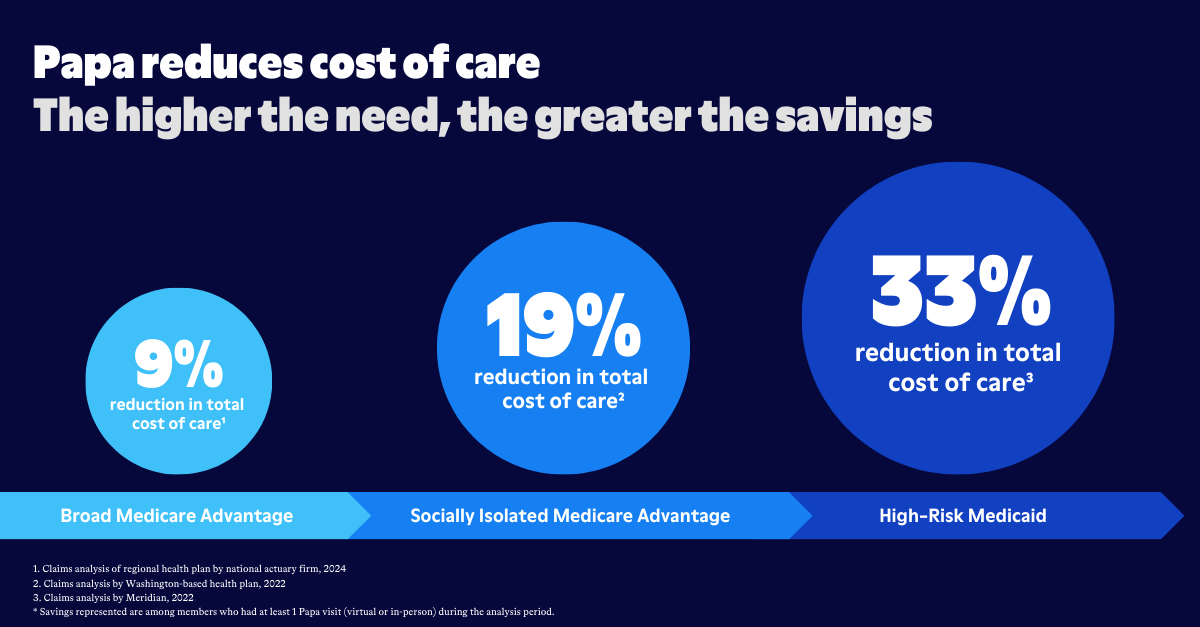
Just like these initiatives, Papa was also born out of a felt need in the community and a desire to address social determinants of health. Andrew, Papa’s CEO, and his family were struggling to balance daily life with caring for Andrew’s grandfather, “Papa.” They knew that so many others in their community—and across the country—shared this struggle and could benefit greatly from companionship and help. In 2017, Papa (the company) and Papa's companion care services that support Medicaid members were born.
Here are several more programs and services Medicaid health plans are providing to people who need them most:
- Referral systems for food assistance
- Free or reduced internet service
- Flexible housing pools to address racial inequities in homelessness
- Non-emergent transportation to grocery stories, pharmacies, etc.
- Diabetes management education
- Maternal home visiting programs
- Exercise bikes for people with developmental disabilities
- Community resource fairs
- Virtual wellness workshops
- Community health workers recruitment, training, and mobilization
- Retinopathy screening at routine PCP visits
- Telemedicine and digital engagement
- Bilingual/bicultural behavioral and mental health services
- Midwifery models of holistic care
- And so many more
It’s easy to feel discouraged and overwhelmed by the pandemic and all the ways it has made life harder for so many people, but we can be encouraged by all of the creative innovations Medicaid health plans have implemented to help fill a wide variety of needs.
The pandemic brought inequities front and center, and Medicaid health plans have risen to the challenge with innovative programs and benefits for their most vulnerable populations. They have demonstrated the power of asking communities about their most pressing specific needs, and they are and coming together to take action in new and imaginative ways. Social determinants of health have a significant impact on the overall health of individual communities and the nation as a whole, and these health plans are committed to addressing them.
As we move into this new and unprecedented post-pandemic world, Medicaid health plans are leading the way toward equity and flourishing health for all.