In a post-pandemic world, we have come to realize that health starts in the home like never before.
When people think of care at home, they often think of telehealth appointments—and that’s definitely a part of it. But in recent years, there has been a real shift in what care in the home can look like.
Last month, at our Papa Pathfinders Summit, a group of health care professionals including the CEO of Care Oregon, Eric Hunter, Dr. Ray Dorsey from the University of Rochester, and Kelsey McNamara from Papa discussed how health care is shifting to the home. (Watch the entire session here.) During the session, we learned a lot about the factors that are driving health providers and health plans to offer health care services that are on the member's terms, and provided on the member's turf.
Home-based health care solutions put people first
As health care providers, we work hard to care for people in ways they want to be treated, not just the ways we think they should be treated. But how do we know how they want to be treated?
We listen to them.
We ask them what matters most to them, what would make them feel best cared for, and then we make every effort to give them what they want and need. Why would we force people to be cared for on our terms, not theirs?
Health care providers can offer care directly to patients in their home, and they have ways to monitor their progress at home. Papa and other organizations provide yet another way to care for people where they’re at. It starts by asking them “what do you need most?”
Maybe the member needs help picking up prescriptions or healthy food. Or perhaps they need help making sure that there aren't safety hazards in their house or that the walkway is de-iced. Maybe they need someone to help them schedule a doctor's appointment or a Zoom call.Maybe they just need someone to talk to.
In the simplest of terms: we ask; we listen; we serve.
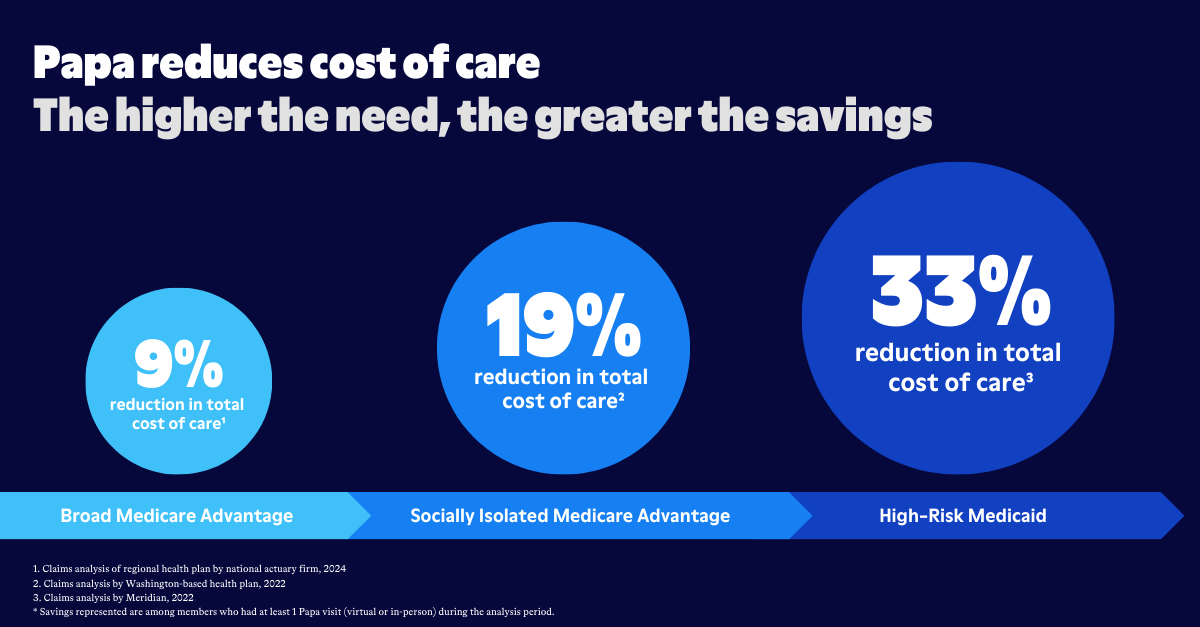
If it seems a bit counter-intuitive to you that something simple like running errands or helping with technology can be part of treating someone's health, recent data has shown that this type of care can pay huge dividends in a member's overall health.
For example, 40% of people who are re-admitted to the hospital claim that a factor at home, such as the inability to pick up a prescription or cook a meal, contributed to their readmission. Additionally, members who get social support have demonstrated a 50% increase in cancer screenings, and a 25% decrease in ED visits. The data has shown again and again that social support leads to better health outcomes.
By moving health care to be more member-focused, you create a culture where each member's needs are not only heard, but met.
Why do we think the best care is provided in a clinical setting?

Where did we get the idea that a clinical setting is the best place for a person to receive health care? For the most part, it’s something we’ve just accepted over the years. But we need to challenge this assumption, because so often, it’s not true.
It requires a lot of time, effort, money, and transportation for someone to get to a clinical setting for care. Most office hours (8-5 Monday through Friday) aren’t sufficient. A lot of people need care in the evenings and on weekends. And the fees-for-services system is not ideal. What if payment was tied to outcomes instead of isolated services that may or may not be helpful?
There are many reasons to choose home health care over a hospital environment.
- It’s less expensive
- Being comfortable results in quicker recovery
- Freedom and normalcy and minimal interruptions
- Reduced exposure to other illness
Preventive care has been proven to save so much unnecessary spending—by decreasing ER visits and Medicaid costs. It also prevents unnecessary illness, depression, and even death in some cases.
What if hospitals existed for trauma care, and everything else we could head off at the pass?
Obstacles to (and limitations of) home health

So we know that most adults prefer to receive care in their own home, but there are things that can get in the way of that.
The first possible barrier is the person’s home itself. (For the purposes of this article, let’s assume the person has a home. We will address housing instability at another time.) At Papa, we have an advantage over health care providers who never see inside a person’s home. Papa Pals are able to assess an older adult’s living conditions to see if they’re appropriate for them to age in place and/or receive home health care.
We can observe and answer questions like:
- Is there dust?
- Does the heat (and/or A/C) work?
- Is there mold?
- Are stairs/railings safe?
- Are necessary items easy/safe to reach?
- Are the rooms in the house accessible to the member?
- Is the neighborhood safe?
- Do they have all the equipment they need?
This is a very incomplete list, but assessing things like this can help determine if the home is safe and appropriate. Do changes/modifications need to be made? Are they feasible/affordable? Being in someone’s home is such a valuable tool to help us see what’s really happening.
Other limitations include (but are not limited to): caregiver burnout, serious medical situations, and expensive out-of-pocket costs if the person’s health care plan doesn’t cover care at home.
Let’s get innovative about caring for people at home
The COVID-19 pandemic changed health care forever. Necessity is the mother of invention, and the pandemic forced us to get creative with health care—and fast. When we had to, we made do with health care at home and via mobile devices. And in many cases, it turned out to be better for everyone all around.
One of our biggest challenges is to convince the health care industry and the government that investing in home health care spending upfront will prevent exponential spending down the road. In an ideal world, healthy people and communities would be all that mattered, but we know we have to talk about the “bottom line.”
And the most important bottom line is this: take good care of people in their homes, and this will have a positive impact on society all around. Human health care should not be about quarterly results. This is a long play. We have to dig deep right now if we want to have a massive impact a few years from now.
When it comes to non-health-related aspects of life, people are banking from home, ordering groceries from home, attending conferences from home. The list is virtually endless.
From a health care standpoint, we now do teledental appointments. We can send packets to families who can do fluoride treatments for their kids at home. You can do an EKG on your watch. We’ve got telemonitoring, e-prescriptions, photo-based consultations. This list is endless as well.
There’s even one very exciting “innovation” happening in many places that is actually a throwback to days of old: doctors making house calls.
Yes, home-based health care strategies are a long-term investment. But they’re going to be well worth the cost. As long as we start putting them in place today.