Health plans need to find a way to close the gaps.
Preventive health care improves health outcomes while reducing care costs, but what happens when people don’t go to their appointments or fail to schedule annual wellness visits altogether?
Gaps in care, particularly among older adults, result not because members don’t value their personal health. Instead, they’re usually due to the barriers they face around health care navigation and compliance. The problem for health plans is that these gaps can be expensive—when you don’t have a way to catch conditions early, they’ll only get worse and cost more over time.
The good news is that health care navigation and compliance can be readily addressed by offering companion care as a supplemental benefit. Here’s a look at how companion care services can help health plans by bridging the gap to preventive-care success.
Barriers to better health
With less than a third of Medicare Advantage enrollees receiving an annual wellness visit, the big question on the minds of many plan administrators has to do with the reasons why.
“Getting preventive care,” notes the U.S. Office of Disease Prevention and Health Promotion, “reduces the risk for diseases, disabilities, and death” in people of all ages.
- 1 in 2 older adults need help understanding their insurance benefits
- Less than 30% of Medicare Advantage enrollees receive an annual wellness visit
- 46% of older Americans need help understanding their insurance coverage
So what’s keeping older adults from following the experts’ advice and seeing their providers for preventive services? The answers are as varied as plan members themselves.
- Realizing the importance of preventative health. Some older adults have trouble understanding why they should prioritize annual visits when they feel relatively healthy, while others might fear what their doctors will find and decide that they’re better off not knowing.
- Limiting health conditions. Many older adults have limitations or heath conditions that make it difficult to navigate the health care system. Poor eyesight, for example, can reduce ones ability to drive making it difficult to get to appointments, while a person with memory problems could forget to schedule those appointments in the first place.
- Understanding benefits offered. A significant challenge older adults often face involves making sense of the benefits that come with their health plans. They may not be aware that preventive care is even an option—or they may not know where to go to get it. One recent poll, for example, found that nearly half of older Americans need help understanding their health insurance coverage even after they’ve picked a plan.
Lack of digital literacy. Telehealth is increasingly becoming more popular, especially in the age of COVID. This health care trend could drastically improve health care access for older adults, yet many don’t have access to technology or have limited digital literacy—one survey revealing that 27 percent of older adults don’t use the Internet.

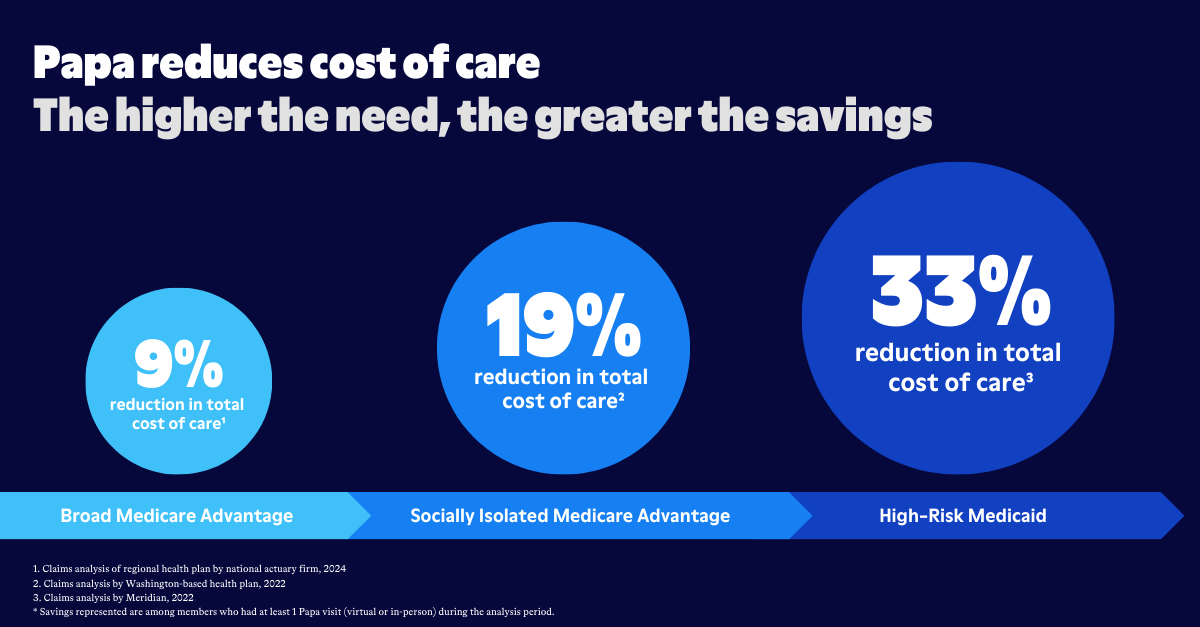
Poor health means higher costs
For health plans, closing these gaps is critical for obvious reasons: Healthier members and lower health care costs.
When people don’t receive preventive services—or follow their provider’s instructions, take their medications as prescribed, or go to other scheduled appointments—they’re more likely to wind up in the hospital or emergency room with serious conditions that are expensive to treat.
In fact, 75% of U.S. health care spending is on chronic diseases that could be avoided through preventive care. Annual wellness visits are associated with a $456 annual cost decrease per member.
Health care navigation: Finding a solution with companion care
Companion care services can help by providing older adults with the support they need to not only understand the health care system. If a member doesn’t understand their insurance benefits, for example, their companion care professional will sit down with them to go over the key points one by one. And if they need help scheduling appointments—preventive care and screenings, follow-up appointments—they’ll get assistance with that as well.
Companion care professionals also typically offer help with transportation, whether it’s to a medical appointment or to the pharmacy to pick up prescribed medications. They serve as intermediaries who speak with administrators when clarification about treatment is needed, and they help members access online resources and telehealth appointments.
Above all else, companion care professionals serve as the “eyes and ears” for the health plan. If there are barriers preventing their client from getting care or services, they’re ready to do whatever it takes to resolve them.
From the health plan’s perspective, they’re there to help beneficiaries avoid the need for potentially expensive interventions. And from the point of view of their members? For them, companion care is about having a friend who’s always available to lend a helping hand.