Papa takes the experience of our health plan partners’ members very seriously.
This is because every member relies on their plans (and us!) for quality care and we are committed to ensuring that care is delivered through the highest possible standards.
At Papa, we value our partnership with Medicare Advantage (MA) health plans and we want to ensure that we support these plans in elevating member experience so that they can align with the values and missions of MA.
In 2022, Medicare Advantage (MA) health plans have a critical goal to elevate their CAHPS™ member experience scores. This is important for the health and experience of the many members who rely on MA, but also in order to achieve top status in Center for Medicare/Medicaid Services (CMS) Star Ratings, which tie directly to CMS bonus and rebate dollars. By working to ensure a high-quality member experience, insurers have the opportunity to differentiate and grow meaningful membership by offering holistic and engaging experiences to succeed and shine in the marketplace. In fact, member experience will be the driving factor for the 2023 CMS Star Ratings.

This is exactly what we at Papa hoped for, because it brings to the forefront the importance of giving members the best possible experience with their health plan and their health care.
At Papa, we have a feedback loop system that helps our partners in health care to monitor member experience in a meaningful way, so that together we can determine areas for improvement and to improve on those so that member experience scores will get better year over year. This not only ensures that we (in alignment with the health plans that we work with) deliver the quality of care that we want to deliver, but that the health care plans that we are part of being able to get the highest ratings. One way that we found to do this is through CMS Star ratings.
How Star Ratings help us (and our partners) deliver quality member experiences
Each year CMS assigns Star Ratings to MA plans to compare quality across health plans on an “apples to apples” basis. For 2023, a maximum of 40 quality indicators that broadly measure effective preventive medicine, member health, and member experience comprise the Star Ratings system.
Customer-experience-related metrics will dominate overall MA Star Ratings. Here’s are some key insights:
- Patient Experience and Complaints measures will constitute 42% of total Star Ratings in 2023, a 45% increase from prior years.
- The primary driver of this significant change is the CMS increasing 8 out of the 9 Consumer Assessment of Health Plans/Providers Services (CAHPS) measures to four weighted measures.
- This increase reflects CMS’s commitment to put patient needs first and empower them to work with their health plan providers to make timely, informed and patient-centric health care decisions.
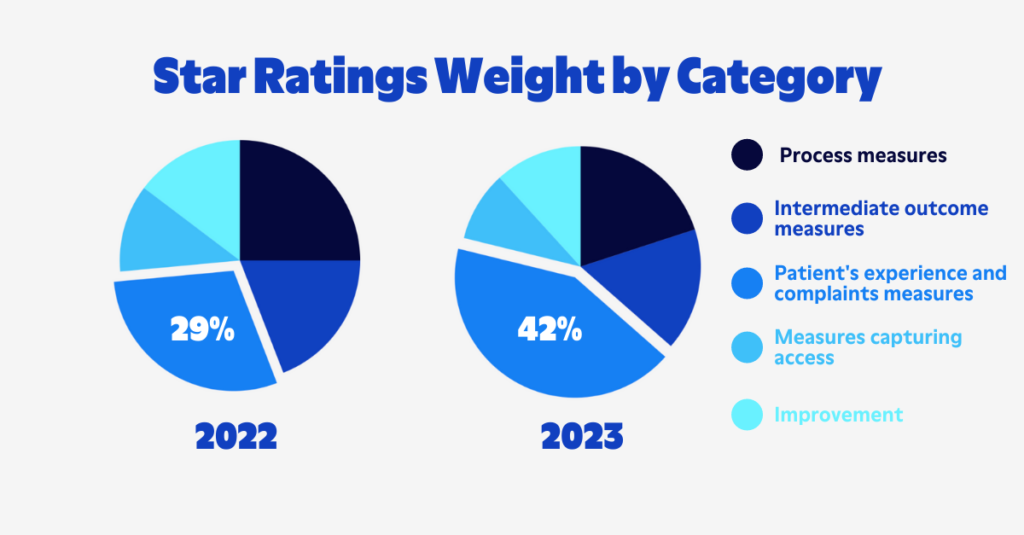
When comparing, crossing a star measure cut point in any of these four weighted measures will have a sizeable impact on a plan's five-point STAR Rating. Historically, the health plan sector is one of the lowest-performing sectors for customer experience, only surpassing the utilities sector in customer satisfaction.
What can you do to ensure continuous improvement and funding?
Interestingly, because of the way health plans are rated and funded based on member experience, the standard of care delivered often directly impacts funding.
Health plans that once had more than 4 stars, but didn’t measure high in customer experience in the most recent ratings, are at risk to decline in Star Ratings. Not only will plans have to maintain customer experience, they will have to improve, as other plans will focus on improving their scores, thus shifting cut points.
When comparing the performance of all quality indicators in 2021-2022, 7 out of the 8 CAHPS member experience measures increased in performance. With CAHPS scores increasing to four weighted in 2023, health plans can only expect a greater focus on customer experience.
Poor/lowered Stars Ratings have significant financial consequences to health plans—dropping from 4.5 to 4.0 Stars can amount to a loss of $8 per member per month in rebate dollars. The financial impact of dropping from 4.0 to 3.5 stars is even more significant. Plans that drop from 4.0 to 3.5 will lose the 5% Quality Bonus Plan which equates to an average of $45 per member per month in reinvestment dollars.
Essentially, the data shows that dollars reinvested into the health and well-being of members through expansion of supplemental benefits and other important features of the health plan will improve quality indicators, attract more new members, and retain existing members for years to come. This not only helps these health plans to better serve their customers, but to get higher ratings and ultimately, more funding.
Is there a downside to tracking member experience through CAHPS?
CMS Star ratings aren’t a perfect system or the end-all in determining member experience.
CMS requires health plans to administer the CAHPS survey annually through a certified vendor. The surveys are released to a random sample of the MA plans membership between February through April of each year. This annual survey sampling creates a barrier for health plans to know on a real-time basis how their members view the health plan; they are unable to mitigate members who are not experiencing exceptional service before the report comes out.
A more holistic approach where health plans would have the option to improve member experience would likely move the needle on member experience even more.
Another downside to the CAHPS member experience data is that it leaves health plans with few options for improvement. Data shows that mailers, phone calls, and member incentives aren't enough to improve the customer experience with their health care and health plan. Health care and health plans are often confusing to older adults. The National Assessment of Health Literacy reported that only 3% of older adults are proficient in health literacy, including health care and plan navigation and understanding health information.
Because of this, many health plans seek alternative ways to improve star ratings and to ensure that their members get the best possible care.
Papa’s take on member experience and quality care
Like we said earlier, at Papa, we care about member experience.
It’s at the core of what we do.
But it’s also at the core of our partner health plans so it’s doubly important to us.

Because of this, Papa has worked to offer a beneficial approach to help health plans improve their member experience in 4 key ways:
Measurement
You can’t improve what you don’t measure. Papa provides a pulse check of members’ health plan experience throughout the year, giving health plans real-time data so that they can make continuous improvements. This information ties directly to a member’s experience with the health plan or network provider and will inform the health plan of any key improvements or necessary adjustments before the annual CAHPS survey is sent.
Personalized Engagement
Papa personalizes the experience and correlates it to distinct member experience measures. Through regular assessments of our members and feedback from our Papa Pals, we examine data on what our members need most, calculate our proprietary Papa Social Index score for each member, and personalize members’ experience based on their PSI score. All of these activities and services correlate to specific member experience measures.
Resolution
Papa’s care concierge service follows up with members who state a poor or average member experience either through assessments or through communication with Papa Pals. Care Concierge staff are trained to:
- listen to the member
- understand any issues
- assist with resolving potential grievances
- report the issue back to the health plan
Reminders
A gentle reminder goes a long way. Papa Pals and Care Concierge Care Navigators are trained to remind members that if they receive a satisfaction survey in the mail or through outreach with a phone call, to please complete it. 4.5 and 5-star plans oversample their membership in order to capture as many responses as possible, which usually slightly favors positive responses, and allows us to learn more about their membership through post analytics.
Rather than waiting for the annual survey results to understand your members' needs, Papa Pals and Care Concierge can provide high-touch services, reminders, and experience check-ins to improve members’ experience perceptions, improve response rates, and inform the health plan for better outcomes.
Member experience is an important component in ensuring quality care, and it will drive Star Ratings this year and beyond.
Focusing on experience is an opportunity for health plans to make sure they are serving their customers with the best quality care in order to improve their Star Ratings, position them as leaders in health care, and increase member growth and retention.