Any Medicare Advantage plan can attest to the traditional ingredients of high-quality patient care: Compassion, talented providers, a commitment to safety and efficiency—for as long as the industry has existed, they’ve all been critical to success.
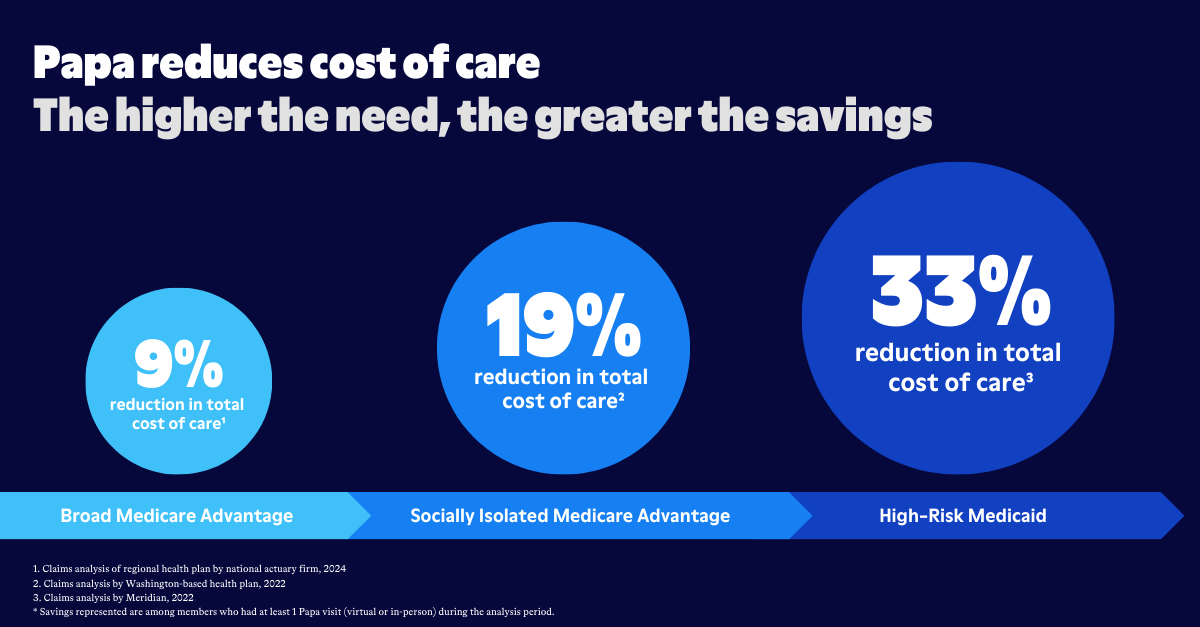
Likewise, the same has been true when it comes to the insurance business itself. Good medicine means healthier people, which in turn is the key to reducing care costs.
What organizations haven’t traditionally considered is their proficiency at addressing the socio-economic challenges that people face. These “social determinants of health,” as they’re known, first came into prominence in the United States following the passage of the 2010 Affordable Care Act, which highlighted the health disparities that often arise from social inequities. Since then, a growing body of research has only added fuel to the “SDoH” fire: Plans that ignore the social determinants of health can expect poorer health care outcomes and higher health care costs.
This is especially the case for health plans that serve older adults, many of whom are at higher risk of poor health and hospitalization because of unmet social needs. From inadequate access to nutritious food to the difficulties that come with maintaining a safe home environment, the SDoH challenges many older adults face are common reasons for increased health care utilization.
So what can health plans do to ensure they come out ahead on the SDoH front? One place to start is by offering members the very social support they require.

Sizing up the SDoH problem
To understand why social determinants are so important to individual health, it helps to consider what life can be like for older adults living alone at home.
Among the frail and those with disabilities, it may be difficult to even get out of the house without assistance from friends or family. Similarly, an older adult without reliable transportation may struggle to get to the store to buy groceries or to make it to the pharmacy or doctor’s appointments. People who are lonely, or socially isolated, may experience mental health challenges. And those who live in homes with unaddressed safety threats may be susceptible to serious injuries.
Compounding the SDoH problem is the fact that three out of four older adults want to age in place. People are living at home into old age because it’s what they know and they value their independence, but many are doing so with little social support, and many wind up paying for it with their health.
By one recent estimate, 80 to 90 percent of the “modifiable contributors” to health fall into the category of SDoH. More than half of older adults, meanwhile, report that they have at least one unmet social need, and one in four say they’re experiencing two or more. The one big change health plans can make to improve the health of their members the most is to provide them with solutions that take the SDoH bull by the horns.
Addressing SDoH with supplemental benefits
While Medicare Advantage organizations have always understood how valuable supplemental benefits are to members, most only recently started investing in benefits that specifically target SDoH.
One recent report by the Better Medicare Alliance found a “dramatic increase in plan activity to address social needs”, especially in the areas of social isolation, transportation, housing, and food insecurity. Overall, the researchers found, the number of Medicare Advantage plans offering SDoH-focused benefits tripled in 2021 alone.
The benefits plans provide to members vary according to the populations they serve, but one increasingly popular offering—because it helps plans identify when social needs are unmet—is companion care.
“Studies have shown that increased levels of social support are associated with a lower risk for physical disease, mental illness, and death.”
-U.S. Department of Health and Human Services

With companion care services, organizations have found, they’re able to differentiate their plans from those of their competitors while directly overcoming SDoH-related barriers. A companion care professional, for example, can provide transportation to preventive screenings their client might otherwise have to skip. They can take them to free community programs like vaccination clinics and health-education events. They can also help them with grocery shopping, whether it’s getting to and from the store or offering assistance finding items in the aisles. And back at home, they can provide a helping hand with everything from light cleaning and organizing to cooking and pet care.
Also in the home, the companion care professional can conduct basic safety checks to ensure there are no tripping hazards, for example. If they notice a hallway is dimly lit, or that the bathtub doesn’t have a mat on the floor, they can resolve these issues in just a few minutes with a trip to the hardware store.
Companion care professionals aren’t health care providers, but they do become trusted friends and companions of the older adults with whom they work. This puts them in a perfect position to recognize when SDoH may be a factor in a client’s life. It also puts them in exactly the right place to make a positive difference in their health—and to help health plans better control health care costs.